Introduction
An accurate diagnosis and proper treatment planning make implant treatment a long term success. Clinical examination and mounted cast models give us information about the maxillomandibular relationship, available space, occlusion, inter-arch distance and relative parallelism. With the help of radiographic examination, the critical landmarks such as the mandibular canal, maxillary sinus, and roots of adjacent teeth are identified. Based on all these findings a workable treatment plan is formulated for the patient, which solves the chief complaint of the patient, provides a good functional and esthetic result and is expected to function for a long duration of time.
The general rules followed during implant placement
Following are the general principles followed during implant placement,
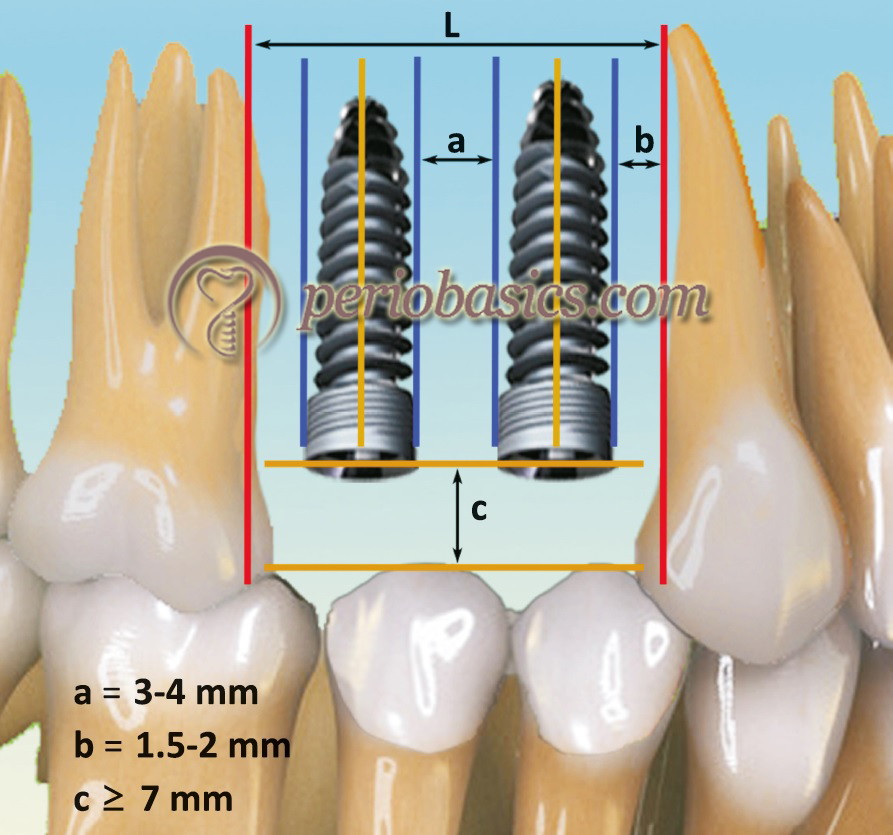
- The minimum distance between the implant margin to adjacent tooth should be 1.5 mm to 2 mm.
- The minimum distance between two implants should be 3 mm to 4 mm.
- Buccolingually, the implant should be placed at 2 mm to 3 mm distance from the cervical height of contour.
- Coronoapically, the implant should be placed at 2.5 mm to 3 mm from the bucco-gingival margin.
- At least 7 mm of inter-occlusal/inter-arch space should be available from the shoulder of the implant to the occlusal surface of the opposing tooth.
- A buffer zone of 2-3 mm from the inferior alveolar nerve or floor of sinus from implant apex should be maintained.
These rules should be followed while planning the position and number of implants for a patient. Before we go into the details of the treatment planning let us first discuss the types of fixed and removable prosthesis used with implant mediated rehabilitation.
Types of prosthesis
Depending on various factors discussed in the previous section, a prosthesis is designed for the patient. It must be remembered that the number and position of the implants will be determined by the type of prosthesis that the patient will be restored with. Misch 1 describes the prosthetic restorations into five types. He has divided the prosthetic restoration into two groups: permanent restorations and removable restorations. He described them as FP (Fixed prosthesis) and RP (Removable prosthesis) as described in the following table,
Fixed prosthesis:
FP-1
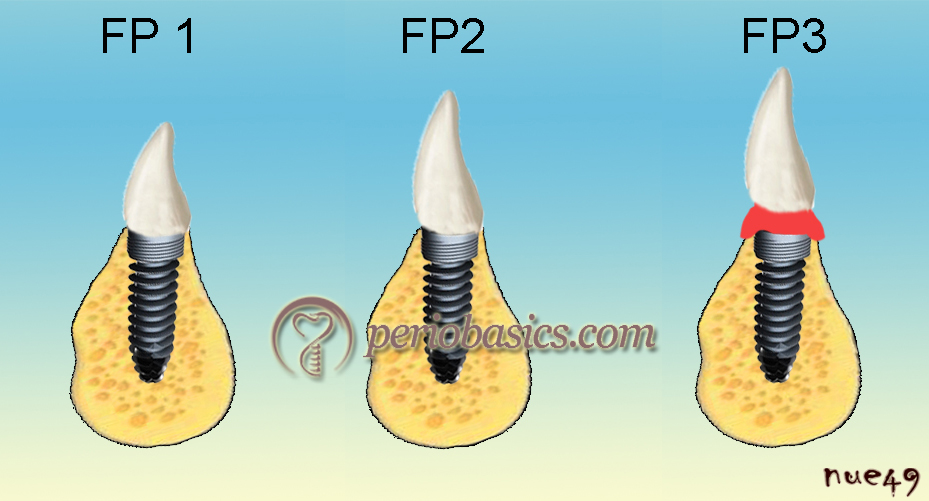
FP-1 fixed restoration is the most favorable replacement of the tooth by an implant form functional as well as esthetic point of view. Especially in the maxillary anterior area where the esthetic is a prime concern FP-1 fixed restoration provides very good results. In this situation, the remaining alveolar bone is sufficient to allow the placement of the implant in almost the same position as that occupied by the tooth.
| Prosthesis Type | Description |
|---|---|
| FP-1 | Permanent prosthesis, which replaces only the crown. It looks like a natural tooth. |
| FP-2 | Permanent prosthesis, which replaces the crown and a part of the root. A natural contour of the crown can be observed in the half-occlusal third, but it is seen elongated or hyper outlined in the cervical or gingival third. |
| FP-3 | Permanent prosthesis, which replaces the crown, tissue and lost bone, the prosthesis uses denture teeth and acrylic gum. |
| RP-4 | Removable prosthesis, overdenture fully supported by implants. |
| RP-5 | Removable prosthesis, overdenture supported by soft tissue and implants. |
Some problems associated with the anterior maxilla are the width of the crest is less, as well as the interdental papillae, are lost after extraction. To re-achieve the exact shape and contour bone augmentation and papilla reconstruction may be required.
FP-2
In this case, fixed restoration replaces the crown as well as some portion of the root of the natural tooth. Usually, sites of extraction showing a moderate bone loss as well as soft tissue loss can be restored by this kind of restoration. The incisal portion of the crown is in the correct position, but the cervical portion is overextended apically and lingually to the original tooth. It is done in cases with a high lip line where the cervical portion of the teeth is not displayed during smiling or speaking. The patient should be clearly told about this before going for implant placement.
FP-3
Advanced bone and soft tissue loss create both functional as well as esthetic concerns. In this kind of restoration, the prosthesis replaces both the tooth/teeth as well as the soft tissue structures. It is also indicated in those areas where the patient has a high maxillary lip line during smiling or a low mandibular lip line during speaking and FP-2 prosthesis has esthetic concerns. A metal porcelain structure is made with gingival toned porcelain used in the gingival portion. Meal framework can also be used as the superstructure for placing denture teeth and acrylic. This kind of prosthesis is usually called as a hybrid prosthesis.
This prosthesis is complicated to fabricate, especially in edentulous cases where 6-10 implant-supported prosthesis has to be given. Most important is the accuracy of fit of the metal framework on the implants. If there is improper fit, it may cause the undesirable distribution of occlusal forces as well as lateral forces on some implants causing ……Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Removable prosthesis
RP-4
This type of removable prosthesis is totally supported by implants and/or teeth. In the most commonly used design, the implants are splinted by a metal bar or connector. The denture contains the attachment for this bar on its tissue surface. The prosthesis, when inserted, is rigid and totally rests on the metal framework. The placement of the implant should be conducive for the prosthesis. In this case, usually, the implants are placed more lingually and apically as compared to FP-1 and FP-2 design. In the mandible, usually 5 implants are placed in the inter-mental region and in maxilla 6 implants are placed up to the anterio-inferior border of the sinus to support this kind of prosthesis.
RP-5
It is implant as well as tissue supported prosthesis. It is usually planned in cases of advanced ridge resorption, where totally implant supported prosthesis cannot be given. In the mandible, two or three implants are placed in the inter-mental region. These implants may or may not be connected to each other. The ball abutment attachment has been used widely in such cases. The problem with this attachment is that it becomes loose with due course of time. A new system known as “Locator attachment” has been introduced to overcome this problem.
Determination of number and positions of implants
In the case of missing single tooth or a few teeth, the number and positions of implants can be easily determined. As a general rule for all partially edentulous situations in excess of the replacement of a single tooth, the minimum number of implants used should be two. The maximum number of implants to be used depends on the number of teeth to be replaced. Usually, one implant should replace one tooth. As described above, most of such cases require FP-1 or FP-2 restoration. Some cases with advanced bone and soft tissue loss may require an FP-3 prosthesis. How to determine the number and positions of the implants has been discussed later in this article.
It is comparatively easy to restore partially edentulous maxilla or mandible, but, when fully edentulous maxilla and/or mandible is rehabilitated with implants, we must take into account several factors which include:
- Anatomy of the residual bone.
- Quantity and quality of the residual bone.
- Type of prosthesis.
- Number of implants.
- Occlusal forces.
- Antagonist.
- Inter-dental arch relationship.
Treatment planning for fully edentulous maxilla
The amount of bone resorption in completely edentulous maxilla plays an important role in choosing the type of prosthesis. As the resorption of the residual alveolar ridge advances, the distance between the opposite residual ridges increases. When a patient presents a distance greater than 15 mm, the most indicated prosthesis is a removable type (overdenture), as we are able to compensate for the lost tissues using acrylic. If in such a case, permanent restoration of metal porcelain type is used, it can result in the production of elongated teeth, which give an unesthetic appearance.
In such cases, the FP-3 type of prosthesis is designed. Here, hybrid prosthesis using an over contoured metal structure with acrylic and conventional denture teeth is fabricated. The crown, tissue and lost bone are replaced by useing denture teeth and acrylic gum. To effectively distribute the occlusal forces bilaterally, 6-10 implants are distributed according to the shape of the ridge.
Misch has elaborated the distribution of implant on a completely edentulous maxilla according to the shape of the residual alveolar ridge. The maxillary arch can be square, ovoid or conical in shape.
Square shaped arch:
In this shape, the central and lateral incisors do not present a marked facial cantilever, as compared to canines. Less occlusal forces are distributed in the anterior region and implants at canine region can well distribute the forces. So, Misch indicates a minimum of two implants in the canine position.
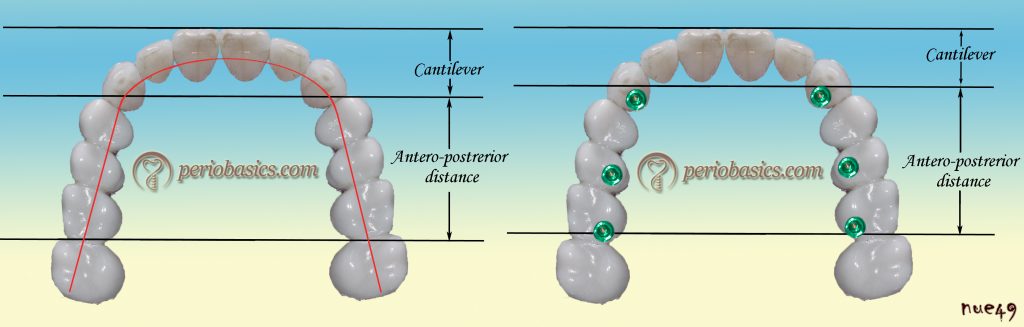
Ovoid shaped arch:
In the case of ovoid arch, more forces are distributed in the anterior maxilla. A minimum of three implants in the premaxilla, two in the position of the canines and one in the position of central or lateral incisors are indicated here.
Conical shaped arch:
This is the most challenging situation because of the high occlusal force distribution in the anterior part of the maxilla. In this case, a minimum of four implants in the front section are indicated, two in canine position and two in the position of the central incisors.
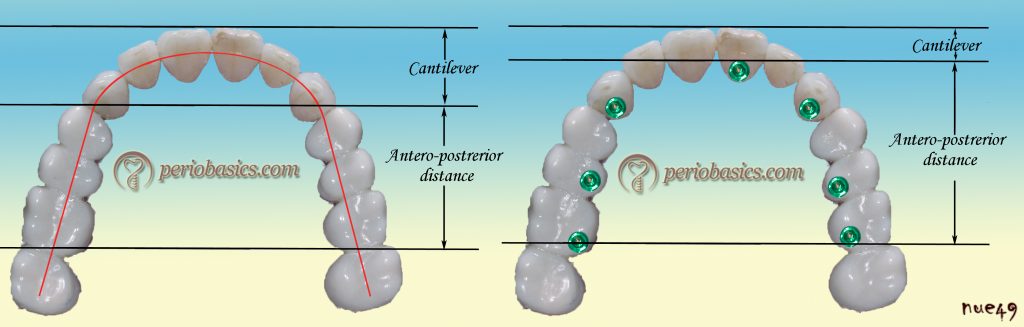
Treatment planning for fully edentulous mandible
As discussed in the case of maxilla, mandible also has three types of arch forms:
- Square shaped arch.
- Ovoid shaped arch.
- Conical shaped arch.
Usually, in the case of advanced resorption RP-4 or RP-5 prosthesis are designed. If implants can be placed in the posterior areas of the mandible, FP-3 prosthesis can also be designed for the patient. In the case of removable prosthesis, most important measurement is the anteroposterior spread of the implants. As a general rule, when 5 implants are placed in the anterior mandible between the mental foramina, the cantilever should not exceed ……Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
How to make a treatment plan
Decisions have to be made regarding the treatment plan according to the patient’s clinical presentation, to deliver a prosthesis which is expected to last long and fulfills patient’s desires. The patient may be partially or fully edentulous. In both the cases, the basic principles of implant therapy have to be followed. Following is the description of various factors which have to be considered during making of a treatment plan,
To retain or extract a natural tooth:
On examination, the teeth are examined for their health status. According to Misch 2 if a natural tooth has a prognosis of more than ten years, it is included in the treatment plan and if it is in the range of 5-10 years, an independent implant-supported prosthesis is advised. If the prognosis of the tooth is < 5 years, extraction of the tooth and bone graft placement is advised so that implant placement after healing can be done. A tooth with good periodontal support can be utilized as an abutment for tooth and implant supported prosthesis. Teeth with poor long-term prognosis, such as, repeated failures with endodontic treatment, root canal anatomy that do not allow the tooth to be restored by post and core treatment, tooth associated with periapical pathology can be considered for extraction.
Immediate implant placement:
The implant can be immediately placed in an extraction socket. Several studies have documented the high success rate of immediate implant placement 3, 4. However, in the posterior maxilla immediate implant placement is frequently complicated by the absence of adequate quality and quantity of the bone and presence of maxillary sinus. Augmentation of sinus floor is indicated to achieve an adequate volume of the bone for proper implant stabilization.
Immediate implant placement in the maxillary and mandibular anterior region has esthetic concerns. New implant materials and designs have helped us in achieving this goal, but an accurate surgical procedure, as well as implant placement, is a must to achieve the desired results.
Number and location of missing teeth:
The number and location of missing tooth/teeth play an important role in the determination of the treatment plan. It is generally accepted that implant therapy in the esthetic zone is a challenging task. A lot of factors have to be considered while placing the implant in the esthetic zone, which includes volume of the bone available, soft tissue profile, angulation of implant for best esthetic results, and buccolingual placement of the implant.
Implant placement in maxillary and mandibular posterior areas may be challenging when adequate bone is not present. In such cases, bone augmentation is required to provide adequate support to implant. Maxillary bone is porous as compared to the mandibular bone because of which achieving primary stability is difficult especially when bone available is minimal. The maxillary sinus uplift procedure is carried out to increase the volume of bone to achieve adequate bone support for the implants.
Implant only supported or tooth and implant-supported prosthesis:
It was historically believed that if a tooth and an implant were used as abutments in the same prosthesis, the implant would be subjected to an increased bending moment because of differences in their mobility patterns. Because of these forces, the success rate for a tooth-implant-supported prosthesis (TISP) was proposed to be less as compared to an implant-only supported prosthesis (ISP) 5-9. In patients with parafunctional habits like bruxism occlusal forces are even more deleterious to the implant. But there are multiple benefits of using tooth with the implant to support a prosthesis. These include,
- Splinting teeth to implants provides more treatment options, especially, when anatomic limitations restrict insertion of additional implants (e.g., maxillary sinus, mental foramen), when the bone is lacking for implant placement and when patient refusal to undergo a bone augmentation procedure.
- Teeth provide proprioception, so a natural tooth-like perception can be enhanced.
- Additional support for the total load on the dentition.
- Reduction of the number of implant abutments needed for a restoration and hence reduced cost.
- A need for cantilever may be avoided by using the tooth as support.
Because of the biomechanical problems associated with the tooth-implant-supported prosthesis, many authors have advocated the use of a nonrigid connector or telescopic crowns to reduce the bending moments on the implant 10-18. But, the problem associated with this treatment is the intrusion of involved tooth/teeth. Surveys indicated intrusion occurred, on average, in 3% to 5.2% of the cases 17, 19. Another option proposed is the use of conventional fixed partial denture. In spite of all the complexities involved, the tooth-implant-supported prosthesis can be used if the following factors are kept in mind before planning the treatment,
- Only those teeth, which have good periodontal health and dense bone support should be used.
- Rigid connectors should be used most preferably in one piece casting.
- The parallelism between the implant and the tooth is important to efficiently distribute the occlusal forces.
- Permanent cementation should be used.
- Only short span bridge should be planned whenever possible.
- This kind of prosthesis should be avoided in patients with parafunctional habits.
- Patients with high caries index are not good candidates for this treatment.
- Occlusal harmony with the opposite arch is a must and there should be an efficient load distribution in the opposite arch.
- Endodontically treated teeth with insufficient occlusal structure or teeth with unsatisfactory treatment should not be included in the treatment plan.
Visibility of the residual ridge crest:
Visibility of the residual ridge crest is usually associated with the amount of bone loss. The visibility is more common with minimal bone loss. In advanced bone loss (Division C and Division D), the residual ridge is not usually visible and the treatment plan is changed accordingly. In the case of minimal bone resorption, there is a tooth-only defect and a metal-ceramic prosthesis may be designed. But, in the case of advanced bone loss, there is a composite defect which requires replacement of tooth as well as soft tissue. The detailed description of the type of prosthesis has been discussed later.
Lack of vertical dimensions of occlusion (VDO):
Due to the loss of posterior teeth, the posterior stops are lost which can lead to bite collapse. In such situations, the vertical dimension at rest position is measured and the interim prosthesis is given to open the bite in harmony with the temporomandibular joint functions. This situation is further complicated by the supra-eruption of the teeth in the opposite arch which further reduces the inter-arch distance. If after opening the bite to its desired vertical dimensions, inter-arch space is still insufficient to place implants; intentional root canal treatment of supra-erupted tooth/teeth and positioning of crown/bridge in the desired vertical position is recommended.
Planning for implants becomes further complicated by the presence of conditions like combination syndrome. Combination syndrome is a condition in which edentulous maxilla is opposed by natural mandibular anterior teeth, presenting with loss of bone from the anterior portion of the maxillary ridge, overgrowth of the tuberosities, papillary hyperplasia of the hard palate mucosa, extrusion of the lower anterior teeth, and loss of ……Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Planning for a cantilever
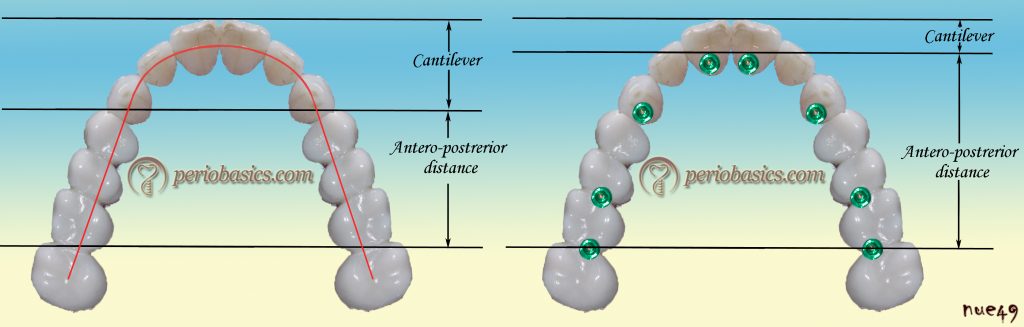
As already explained, when planning a treatment for the edentulous mandible, cantilever prosthesis can be designed depending on the total implant support as well as the shape of the ridge. Long-term clinical studies have demonstrated that implant-supported full-arch reconstructions with bilateral cantilevers in the mandible exhibited high survival rates 21-23. However, it has been suggested that certain cantilever lengths may decrease the survival of the prosthesis 24.
The conical/tapered shape of the ridge is more suitable for distal cantilever as the anterior implants are able to offset the distal cantilever force. The anteroposterior length of the cantilever can be determined by calculating the distance from the center of the most anterior implant to the line joining the distal aspects of most distal implants. The length of the cantilever should not be more that two and one-half times of the measured anteroposterior distance between the anterior and most posterior implants.
Overloading of the implants should be avoided as it can be attributed to clinical complications such as screw loosening or fracture, fracture of the veneering material, prosthesis and implant fracture as well as implant failure 25-28.
Know More…
Planning an implant in the esthetic zone:
Implant placement in the esthetic zone, that is, maxillary and mandibular incisor area has always been a challenge to the dentists. There are multiple variables that should be considered while planning an implant in the esthetic zone. These include,
Emergence profile: The emergence profile refers to the portion of the prosthesis that allows the implant to turn into a natural-looking tooth. An excellent emergence profile gives a smooth transition from the circular implant platform to the natural shape of the tooth at the gingival level. One of the important factors that affect the emergence profile is the three-dimensional (3D) placement of the implant fixture into the alveolus. If the implant is placed too coronally, there won’t be sufficient length or “running room” (the apico-coronal distance between the platform of a dental implant and the gingival margin) to create an anatomic emergence of the crown from the gingiva.
Implant placement: When placing an immediate implant in the extraction of maxillary central incisor, the placement of the implant should be done more on the palatal aspect of the socket because of differences in the shape of the tooth and implant. A surgical guide should be prepared to accurately prepare the osteotomy site. A CBCT image is useful to evaluate the integrity of the existing facial bone. At least 6 mm gap width in the mesiodistal extension should be there to allow a distance of 1.5 mm or more from adjacent teeth. Also, at least 6 mm buccolingual bone volume should be there to allow 1.5 mm or more on the facial/buccal aspect and a minimum of 0.5 mm on the palatal aspect.
Implant selection: The narrow-diameter implants (those having a platform ~ 3.0 mm) are a good solution for replac-ing mandibular central teeth and incisors, as well as maxillary lateral incisors. A narrower implant will assure at least a 2-mm- to 3-mm-buccal gap adjacent to the intact buccal socket wall. This can be pre-planned with a careful CBCT analysis and an understanding of the restorative-driven plan.
Long-standing edentulous area: If there is a long-standing edentulous area with soft tissue and hard tissue deficiency, hard-tissue and soft-tissue augmentation procedures are recommended to achieve appropriate esthetic results.
Use of surgical guide during implant placement
The fabrication of a surgical guide during implant placement is a very important step in implant therapy. The diagnostic wax-up provides us the information regarding the placement of the teeth and hence the implants. This information has to be transferred/translated via some form of guide to the surgeon during the surgical phase of treatment. For this purpose, a surgical guide is used which is fabricated using information obtained from all diagnostic procedures previously performed 29, 30. With the help of a surgical template, not only the position of fixture/fixtures, but also their correct angulation is achieved.
Indications for surgical template:
- Partially edentulous cases where the alignment of the implants is difficult.
- Full mouth rehabilitation cases where multiple implants are planned.
- Implant placement in areas where important anatomical structures (e.g., maxillary sinus, inferior alveolar nerve) play an important role.
- Used as a carrier when diagnostic markers such as metallic balls have to be placed in the mouth during radiographic procedures to identify the potential implant sites.
There are two types of surgical templates. Same-arch where the template is constructed in the same arch in which fixtures are to be placed and opposing arch where the template is constructed in the arch opposite to the one in which fixtures are to be placed.
Procedure of making a surgical template for the same arch:
After the impressions of the maxillary and mandibular arches are made, the diagnostic casts are obtained and articulated on an articulator. After articulation diagnostic wax-up is done and again an impression is made of the complete arch. The impression is poured and again a cast is obtained with all the teeth in their proposed positions. Using cold cured or heat cured resin a ……Contents available in the book……….Contents available in the book……….Contents available in the book……….Contents available in the book…..
Procedure of making a surgical template for the opposite arch:
The initial steps up to the articulation of diagnostic casts is same for both the procedures. After articulation, the surgical template is fabricated on the opposite arch to that planned for implant placement. The template is constructed using heat-cured acrylic resin or vacuum-molded acrylic resin. The position and angulation for the fixture (i.e., through the cingula or the occlusal surface) is determined. Now, an orthodontic wire is taken and is attached to the template by means of acrylic resin directed in such a way that the opposite end of the wire points at the position of the fixture in the arch where implant placement has to be done. For this, the tooth where the implant has to be placed is removed so that the wire touches the ridge of the arch. During the fabrication of template, the inter-arch distance with the wire should be sufficient to accommodate the hand-piece with a drill during the surgical procedure.
At present, many implant companies have developed computer-guided systems to make surgical templets.
Conclusion
An accurate treatment planning is the cornerstone of successful implant therapy. All the above factors play an important role during decision making regarding size, position, and angulation of the implants. It should be remembered that the final prosthesis plays a vital role in the determination of implant positions. So, a prosthetic wax-up is very useful in treatment planning for an implant case. Whether to retain a natural tooth or to extract it, to give tooth and implant-supported prosthesis, to give cantilever etc. have to be considered during decision making.
References
References available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

